46 YEAR OLD MALE WITH ALTERED SENSORIUM
G SUHITHA GNANESWAR
HALL TICKET NO - 1701006047
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
SHORT CASE:
A 46 year old male came to casuality with chief complaints of
-burning micturition since 10days
-vomiting since 2days (3-4 episodes)
-giddiness and deviation of mouth since 1day
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 10years back, he complained of polyuria for which he was diagnosed with Type 2 diabetes mellitus he was started on OHAs, 3years back OHAs were converted to insulin.
20days back he developed vomiting containing food particles, non bilious,non foul smelling(3-4 episodes),later he complained of giddiness and deviation of mouth for which he was brought to our hospital and his GRBS was recorded high value for which he was given NPH 10U and HAI 10U.
No history of fever/cough/cold
No significant history of UTIs
PAST HISTORY
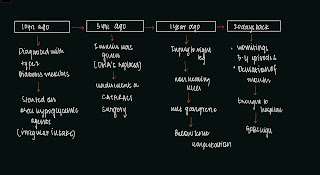
10years back patient complained of polyuria for which he was diagnosed with Type 2 Diabetes Mellitus, he was started on oral hypoglycemic agents(OHA). 3years back OHAs were replaced by Insulin. 3years ago he underwent a cataract surgery. 1year ago he had injury to his right leg, which gradually progressed to non healing ulcer extending upto below knee and ended with undergoing below knee amputation due to developement of wet gangrene.
Delayed wound healing was present- it took 2months to heal
Not a k/c/o Hypertension, Epilepsy,Tuberculosis, Thyroid
Not on any medication
No history of blood transfusion
PERSONAL HISTORY
Diet - Mixed
Appetite- normal
Sleep- Adequate
Bowel and bladder- Regular
Micturition- burning micturition present
Habits/Addiction:
Alcohol-
Not consuming alcohol since 1 yr.
Previously (1yr back) Regular consumption of alcohol, about 90mL whiskey consumed almost daily.Also 1 month on & off consumption pattern previously present
FAMILY HISTORY
not significant
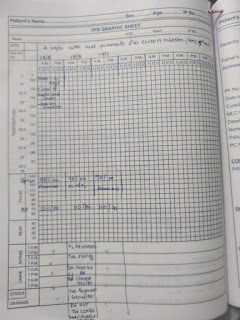
VITALS
Vitals @ Admission:
BP: 110/80 mmHg
HR: 98 bpm
RR: 18 cpm
TEMP: 101F
SpO2: 98% on RA
GRBS: 124 mg/dL
General Examination:
Pallor present
No- icterus,cyanosis,clubbing,koilonychia, lymphadenopathy
No dehydration
CVS: S1S2 heard, No murmurs
RS: BAE+,NVBS
P/A: Soft, Non tender
CNS:
Higher function test:
Pt is having altered sensorium
Slurred speech
Not Orientated to time place person.
Memory couldn't be elicited as pt is in altered sensorium
Cranial nerves : intact
Motor system :
1, Bulk : right. Left
Upperlimb normal. Normal
Lowerlimb. thigh -N. Normal
Below knee amputated on R side
2, Tone :
Upperlimb. Normal. Normal
Lowerlimb. Normal. Normal
3, Power :
Neck:. Normal
Trunk:. Normal
Upper limb 5 5
Lower limb 5 5
4, Reflexes
Right Left
Biceps 2+. 2+
Triceps 2+ 2+
Supinator 2+ 2+
Knee 2+. 2+
Ankle 2+. 2+
Planter reflex Amputated flexion
Sensory system : normal
Meaningal signs : negative
INVESTIGATIONS
ON DAY OF ADMISSION












Comments
Post a Comment